Ki> Payment Integrity
Empowering
Health Insurance
Optimising Payment Integrity

Intuitive, comprehensive, accurate Fraud, Waste, and Abuse detection & investigation
Optimise Payment Integrity with a focus on high-value cases and optimal ROI
Detection Accuracy
Efficiency/ROI
Differentiators
Detection Accuracy
Unrivalled Detection Accuracy
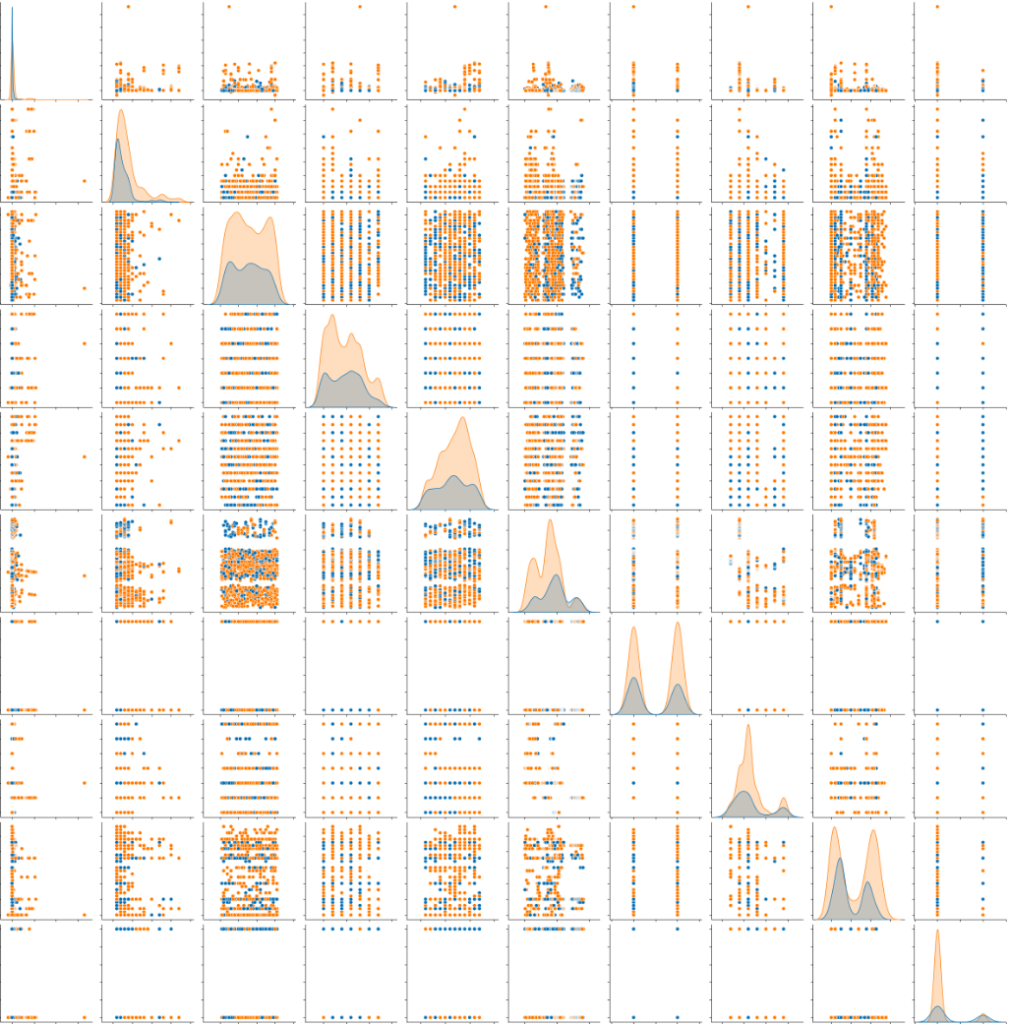
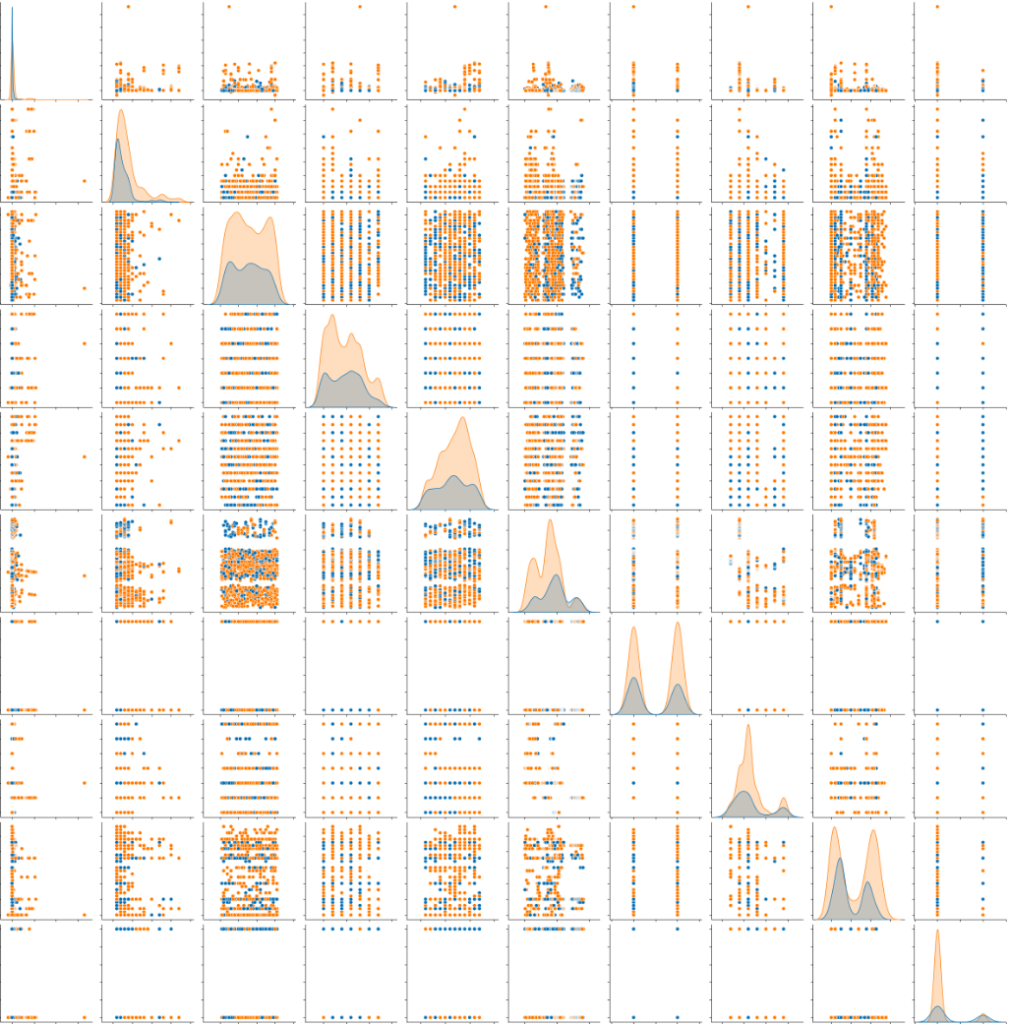
- Unleash Your Data: Kirontech gets your data AI ready by carefully understanding, cleaning, codifying and unifying it. Kirontech then aligns your data with established coding hierarchies so that our algorithms can respond to structures and patterns that would otherwise be hidden.
- Make Fair Comparisons: Kirontech works with your data to refine doctor speciality classifications, creating tight comparison groups that support precise and actionable insights.
Efficiency/ROI
Let Kirontech take you on the journey to 7x ROI
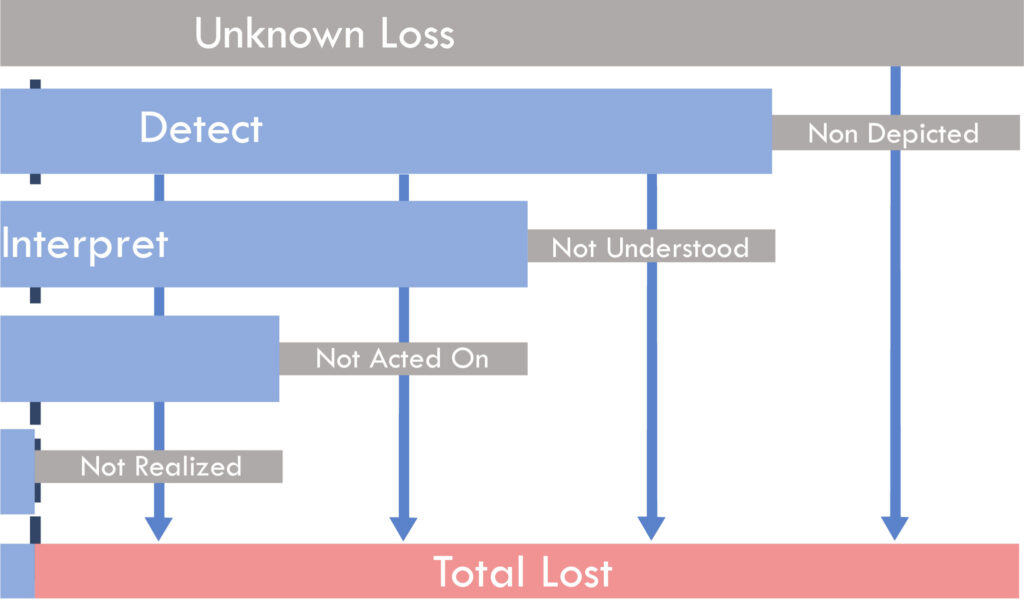
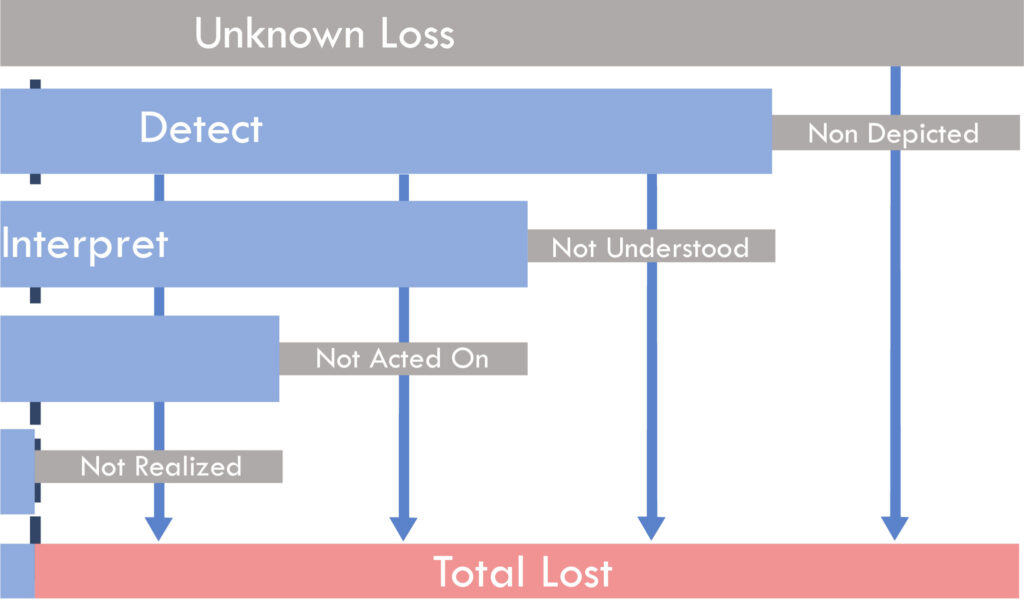
- Show me the Money: Kirontech’s AI detects issues affecting 10%-30% of the claims value. Kirontech gives you a complete view of the intelligence landscape that enables you to release this value.
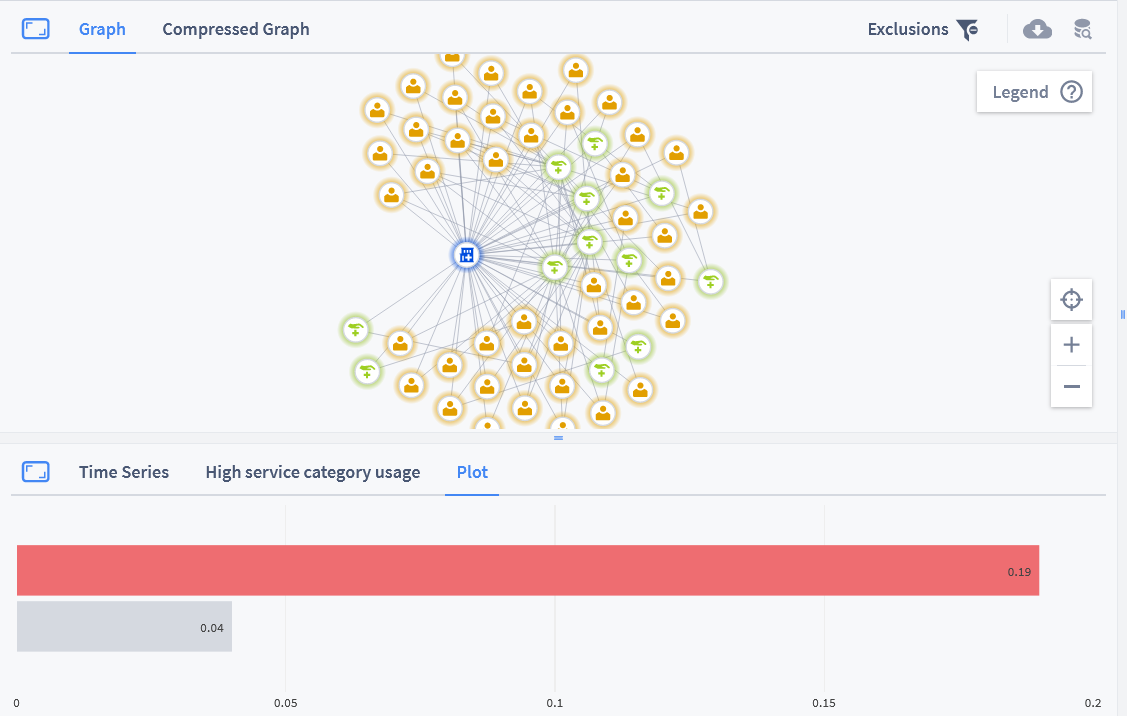
- Efficiency: Our findings provide specific and targeted insights, supported by automatically generated text narratives, data and plots; boosting the efficiency and speed of your team.
Differentiators
Ki> Payment Integrity Differentiators
- Unlocked Hidden Value: Kirontech’s AI considers all the data, finding previously hidden issues at patient, doctor and facility level. Let Kirontech reveal the issues that span claims, either across a patient’s claim history, or across a medical practice.
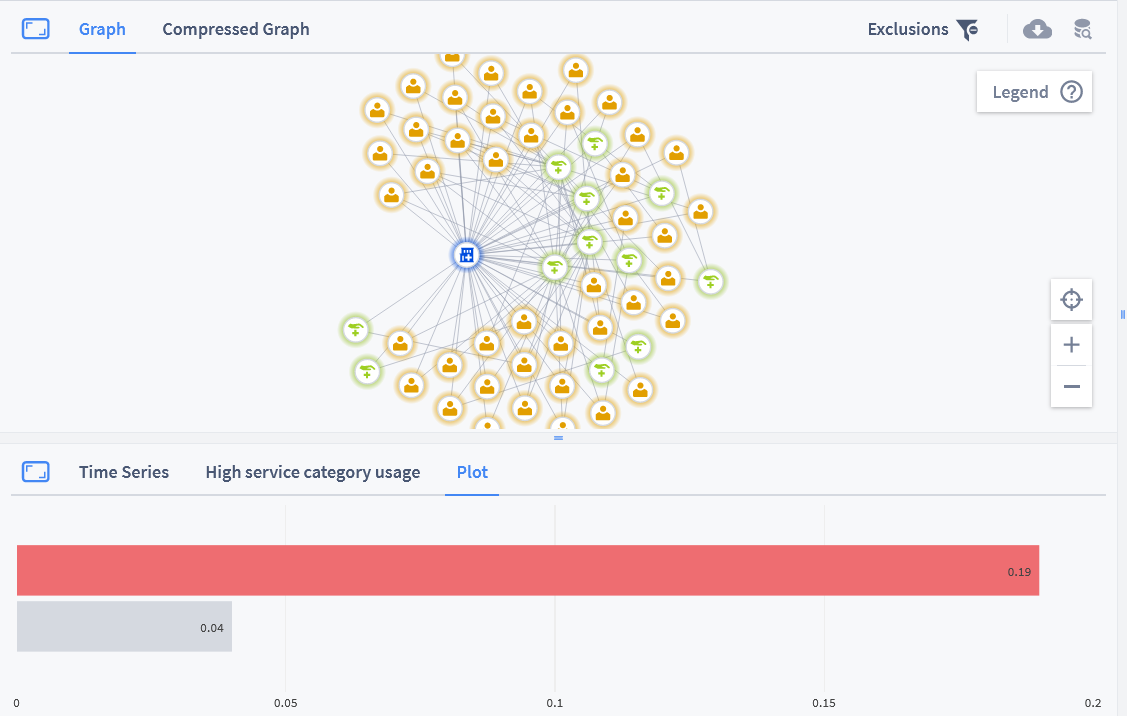
- Trust us to Find Outliers: Kirontech’s AI creates meaningful peer groups to establish regional and market norms and ensure comparisons are fair. Kirontech helps you know where to start, by giving each medical practice an overall risk score.
- Driven by Data: Kirontech AI is driven by a vast array of curated international, regional and proprietary reference data. Kirontech experts continually refine the reference data and tune the algorithms to ensure that they detect issues that are relevant and interesting to you.
- Get the Whole Picture: Kirontech’s pre-built dashboards give you an instant overview of the actors in your data showing you a complete picture of a member, doctor, speciality or provider. Empowering your team with Kirontech’s powerful search, filter, aggregation and plotting tools gives your teams the information needed to qualify and respond to payment integrity issues, saving your company money and time.
Ki> Data
Empowering
Health Insurance
Optimising Payment Integrity & Health Outcomes
Lorem ipsum dolor sit amet, consectetuer adipiscing elit.
Lorem ipsum dolor sit amet, consectetuer adipiscing elit, sed diam
nonummy nibh euismod tincidunt ut laoreet dolore magna.
Tab #1
Tab #2
Tab #3
Tab #4
Tab #1
Unrivalled Detection Accuracy
- Unleash Your Data: Kirontech gets your data AI ready by carefully understanding, cleaning, codifying and unifying it. Kirontech then aligns your data with established coding hierarchies so that our algorithms can respond to structures and patterns that would otherwise be hidden.
- Make Fair Comparisons: Kirontech works with your data to refine doctor speciality classifications, creating tight comparison groups that support precise and actionable insights.
Tab #2
Let Kirontech take you on the journey to 7x ROI
- Show me the Money: Kirontech’s AI detects issues affecting 10%-30% of the claims value. Kirontech gives you a complete view of the intelligence landscape that enables you to release this value.
- Efficiency: Our findings provide specific and targeted insights, supported by automatically generated text narratives, data and plots; boosting the efficiency and speed of your team.
Tab #3
Ki> Payment Integrity Differentiators
- Unlocked Hidden Value: Kirontech’s AI considers all the data, finding previously hidden issues at patient, doctor and facility level. Let Kirontech reveal the issues that span claims, either across a patient’s claim history, or across a medical practice.
- Trust us to Find Outliers: Kirontech’s AI creates meaningful peer groups to establish regional and market norms and ensure comparisons are fair. Kirontech helps you know where to start, by giving each medical practice an overall risk score.
- Driven by Data: Kirontech AI is driven by a vast array of curated international, regional and proprietary reference data. Kirontech experts continually refine the reference data and tune the algorithms to ensure that they detect issues that are relevant and interesting to you.
- Get the Whole Picture: Kirontech’s pre-built dashboards give you an instant overview of the actors in your data showing you a complete picture of a member, doctor, speciality or provider. Empowering your team with Kirontech’s powerful search, filter, aggregation and plotting tools gives your teams the information needed to qualify and respond to payment integrity issues, saving your company money and time.
Tab #4
Improve Patient Experience
- Consistently Crush Low Value Care: Escape the drudgery of annual isolated report-driven low-value care projects with Kirontech’s integrated intelligence platform. Kirontech’s year-round detection helps you keep low value care under control. Kirontech aggregates usage at a doctor and medical facility level, to keep you focused on practices that consistently use low-value treatments.
- Reduce Patient Harm: Let Kirontech help you find medical practices that are overusing test and scanning when compared with their peers. When a medical practice uses tests indiscriminately or on asymptomatic individuals, they run a high risk of generating false positive results. As well as causing the patients distress, incorrect results may lead to unnecessary treatments and patient harm.

Ki> Health Outcomes
Empowering
Health Insurance
Optimising Health Outcomes & Quality

Improve Patient Experience, Control Unsafe Practices, Detect Practice Irregularities
Systematically optimise Health Outcomes & Quality
Control Unsafe Practices
Improve Patient Experience
Finding the Missing Pieces
Control Unsafe Practices
Control Unsafe Practices
- Protect your Patients: Kirontech systematic findings will guide you to medical practices that have an unusual pattern of follow-on corrective treatment, complications, and repetitions. Kirontech’s extensive range of data interrogation tools support your team as they explore and respond to problematic billing.
- See Beyond the Brand: Kirontech drug algorithms work at the active ingredient level, allowing us to establish market norms, even when a mixture of branded and generic drugs are used. Drugs represent a significant cost for many healthcare payers, Kirontech’s integrated approach guides your teams to practices that prescribe drugs in a usual or potentially dangerous way.

Improve Patient Experience
Improve Patient Experience
- Consistently Crush Low Value Care: Escape the drudgery of annual isolated report-driven low-value care projects with Kirontech’s integrated intelligence platform. Kirontech’s year-round detection helps you keep low value care under control. Kirontech aggregates usage at a doctor and medical facility level, to keep you focused on practices that consistently use low-value treatments.
- Reduce Patient Harm: Let Kirontech help you find medical practices that are overusing test and scanning when compared with their peers. When a medical practice uses tests indiscriminately or on asymptomatic individuals, they run a high risk of generating false positive results. As well as causing the patients distress, incorrect results may lead to unnecessary treatments and patient harm.

Finding the Missing Pieces
Detect Practice Irregularities
- Find The Missing Pieces: Kirontech helps you find the practices that regularly deviate from established guidelines. A course of treatment with a step missing can be just as wrong as a course of treatment with redundant steps. Kirontech’s powerful whole-patient-history algorithms can detect missing treatments as well as excessive or unusual treatments. Kirontech gathers missing treatment information at a doctor or medical facility level so that you can be confident you are dealing with systematic behaviour, rather than medically justifiable exceptions.

Contact Us
For a Demo or Trial fill in your details below and one of our representatives will get back to you within 24 hours.
This site is protected by reCAPTCHA and the Google
Privacy Policy and
Terms of Service apply.